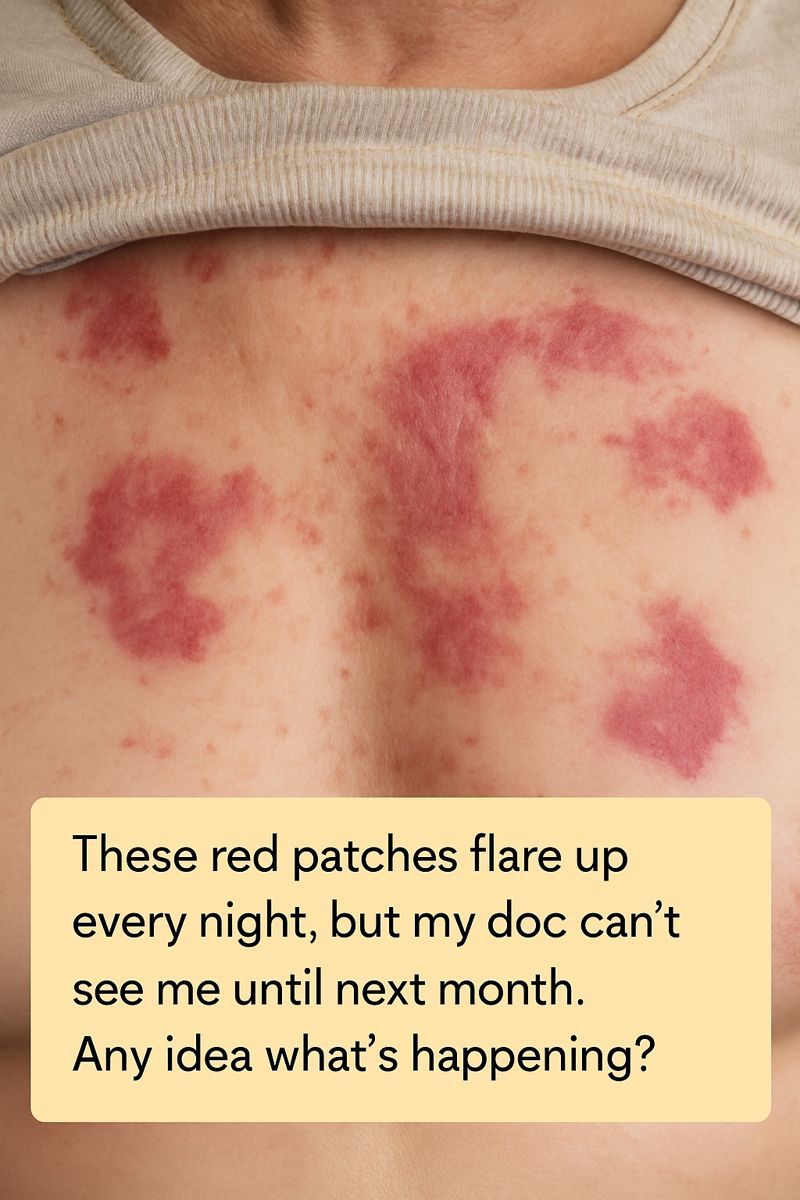
Experiencing red patches on your skin that flare up every night can be both alarming and frustrating, especially when your doctor can't see you until next month. These recurring skin issues can disrupt your sleep and leave you feeling anxious about what could be causing them. While waiting for your appointment, it's helpful to explore potential causes and soothing strategies to manage your symptoms.
Understanding the reasons behind your nightly skin flare-ups can be the first step toward finding relief. From environmental factors to lifestyle habits, many elements could be contributing to this condition. This article will guide you through possible culprits, what to monitor, and how to soothe your skin until you can see your healthcare provider.
1. Why Your Skin Acts Up More At Night
Your skin could be more reactive at night due to the body's natural circadian rhythms. At night, the body's production of certain hormones, like cortisol, decreases. Cortisol has anti-inflammatory properties, so lower levels might make your skin more susceptible to inflammation from irritants.
Additionally, the skin's barrier function can weaken at night, increasing trans-epidermal water loss, which can exacerbate dryness and irritation. This is why some skin conditions, like eczema, often feel worse during the nighttime hours when the skin is less protected.
2. Could It Be Eczema? Classic Signs To Look For
Eczema, or atopic dermatitis, is a common skin condition that can cause red, itchy patches to appear on the skin. These patches might feel dry and scaly, and they are often more pronounced at night. Classic signs include itching that can intensify during the evening and potential oozing or crusting of the affected areas.
While eczema is common in children, it can occur at any age. Genetic factors, environmental triggers, and a compromised skin barrier all contribute to its development. If your symptoms align with these descriptions, eczema might be a possible cause of your nighttime flare-ups.
3. Nighttime Triggers: Heat, Sweat, And Heavy Bedding
The environment you sleep in can significantly impact your skin's condition. Heat and sweat are common triggers for skin irritation. If your bedroom is too warm or if your bedding is heavy and not breathable, it can create a micro-environment that promotes sweating and skin irritation.
Consider using lightweight, breathable materials for your bedding, and keep your bedroom at a cooler temperature to help minimize these triggers. Ideally, the room temperature should be between 60 to 67 degrees Fahrenheit for optimal sleep and comfort.
4. The Role Of Stress, Anxiety, And Poor Sleep
Stress and anxiety can have a direct impact on your skin. Stress triggers the release of inflammatory chemicals in the body, which can exacerbate skin conditions like eczema. Lack of sleep can also place additional stress on the body, making it harder for your skin to recover and repair itself.
Practicing stress-reduction techniques, such as meditation, deep breathing exercises, or gentle yoga, can help manage anxiety levels and improve sleep quality. Prioritizing good sleep hygiene can also support your skin's health.
5. Hidden Irritants: Detergents, Fragrances, And Fabric Softeners
Household products, including detergents, fragrances, and fabric softeners, can contain chemicals that irritate sensitive skin. These irritants might not cause an immediate reaction, but prolonged contact through your clothing or bedding can contribute to nighttime flare-ups.
Opt for hypoallergenic and fragrance-free products, and consider double-rinsing your laundry to remove any residual detergent. Testing new products on a small skin patch before widespread use can also help identify potential irritants.
6. Hot Showers, Harsh Soaps, And Other Daily Habits Making It Worse
Daily habits, such as taking hot showers or using harsh soaps, can strip your skin of its natural oils, leading to dryness and irritation. Hot water can exacerbate the problem by opening up the skin's pores and causing further moisture loss.
Switching to lukewarm water for showers and using gentle, moisturizing cleansers can help maintain your skin's natural moisture barrier. It's also beneficial to apply a thick, emollient moisturizer immediately after bathing to lock in moisture.
7. Food Sensitivities And Allergies That Can Fuel Flares
Food sensitivities and allergies can contribute to skin flare-ups by triggering an immune response that manifests on the skin. Common culprits include dairy, gluten, nuts, and shellfish. If you suspect a particular food might be causing your symptoms, consider keeping a food diary to track what you eat and any subsequent skin reactions.
Elimination diets, conducted under the guidance of a healthcare professional, can help identify specific food triggers. Once identified, avoiding these foods can reduce inflammation and improve skin condition.
8. Viral TikTok Hacks For Eczema: What Actually Helps, What To Skip
TikTok is full of viral hacks claiming to alleviate eczema symptoms, but it's important to approach these with caution. Some popular suggestions, like using aloe vera or oatmeal baths, can be soothing and beneficial for some individuals. However, other hacks, such as applying apple cider vinegar directly to the skin, may cause irritation or worsen symptoms.
Before trying any new remedies, especially those found on social media, consult with a dermatologist or healthcare provider to ensure they're safe and appropriate for your skin type.
9. Over-The-Counter Creams, Ointments, And Band-Aid Fixes
Over-the-counter creams and ointments can provide temporary relief for itchy, inflamed skin. Hydrocortisone cream is a mild steroid that can reduce inflammation, while emollient-rich moisturizers can soothe dry patches.
However, these solutions are often just band-aid fixes. They can help manage symptoms in the short term, but addressing the underlying cause of the flare-ups is essential for long-term relief. Be mindful of using topical steroids for extended periods, as they can thin the skin with prolonged use.
10. When It’s Not Eczema: Other Red-Patch Culprits To Consider
If your symptoms don't align with eczema, consider other potential causes such as psoriasis, rosacea, or contact dermatitis. Psoriasis typically presents as well-defined, scaly plaques, while rosacea often affects the face and presents as redness and visible blood vessels.
Contact dermatitis occurs when the skin reacts to a substance it has come into contact with, causing redness and irritation. Identifying the specific cause will require a proper diagnosis from a healthcare provider, who can recommend appropriate treatments.
11. What To Track Before Your Appointment So Your Doctor Takes You Seriously
Keeping a detailed record of your symptoms can help your doctor make a more accurate diagnosis. Note the timing and duration of flare-ups, any potential triggers (such as foods, activities, or products), and the effectiveness of any remedies you've tried.
Photographing the affected areas during flare-ups can also provide valuable visual information. Bringing this documentation to your appointment can help your doctor understand the severity and pattern of your symptoms, leading to a more informed diagnosis and treatment plan.
12. Safe At-Home Soothing Routines To Get You Through The Month
While waiting for your appointment, adopting soothing routines can help manage your symptoms. Regularly applying a rich moisturizer can help maintain skin hydration. Using a humidifier in your bedroom can also combat dryness in the air, particularly during colder months.
Consider incorporating gentle skincare products with calming ingredients like chamomile or calendula. Avoid scratching the affected areas to prevent further irritation and possible infection. Wearing soft, breathable fabrics can also reduce friction and discomfort. These measures can provide relief and improve your skin's condition until you receive professional guidance.